Photodynamic therapy (PDT) combines the properties of a photosensitising drug absorbed by the skin, and the healing power of light. This therapy is clinically proven as an effective method of eliminating precancerous lesions, sun damage and acne. Photodynamic therapy is a non-surgical, extremely valuable tool that targets damaged and abnormal skin cells.
Photodynamic reaction between photosensitising agents in contact with light and oxygen kills potentially dangerous cancer cells. The technology can be used with various forms of light to provide targeted therapy for smaller areas, or greater scope for large areas of lesion requiring a broader field of illumination. The benefits of PDT are most noticeable when used on sun damaged areas of the skin, including the face, arms and hands.
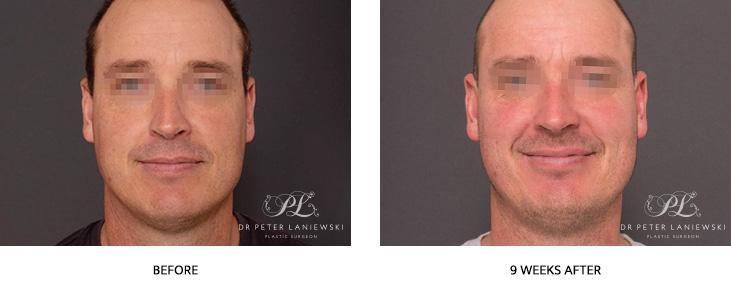
Photodynamic Therapy Photos – Dr Peter Laniewski
PHOTODYNAMIC THERAPY PROCEDURE
Prior to application of the photosensitising agent, the skin needs to be thoroughly cleansed. In some situations, the therapist will perform microdermabrasion, a chemical peel or acetone scrub to maximise penetration. The liquid agent, once applied, needs to incubate and be absorbed for between 30 minutes to 3 hours. When the photosensitising drug solution has absorbed, a light is focussed on the area for up to 20 minutes.
Due to the heat of the light combining with acid contained in the photosensitising drug there may be a sensation of burning discomfort. This can be counteracted by the use of a fan or cold air. Photodynamic therapy has been proven useful in the fight against several varieties of non-melanoma skin cancers including:
- Actinic keratosis: Often occurring on the face and scalp, these are growths that are prone to develop on skin that has been exposed to the sun. Actinic keratosis involves small patches of discoloured skin that can become scaly, crusted or scabbed. They can also itch, sting or burn.
- Squamous cell carcinoma in situ (Bowen’s disease): This early form of squamous cell skin cancer only affects the outer layer of skin, and has not yet harmed surrounding tissue. It is most often found on sun-exposed areas of the body such as face and hands, and appears as sharply defined yet irregular reddish patches.
- Superficial basal cell carcinoma: These are most common on light-skinned people who have been exposed to too much sun. Basal cell skin cancer doesn’t usually spread, and is usually noticed as a small, fleshy lump with a reluctance to heal or disappear. Although not usually dangerous, they can be persistent and reappear after treatment.
AFTER-TREATMENT CARE
The skin will remain very sensitive for a couple of days after photodynamic therapy. Pain will diminish as the medication metabolises. Complete sun protection during initial healing is essential, and wearing a hat, scarf, and high UV sunblock is recommended. Depending on the chemical or cleansing agents used, there could be mild peeling of the skin for two or three days. People with very sensitive skin will experience discomfort for a little longer.
Often, people with the most to gain also suffer greater discomfort after PDT. In other words, for those with a large number of pre-skin cancers, more of the drug solution will be absorbed, resulting in a stronger chemical/light/oxygen reaction. The plus side is that the discomfort experienced is the body’s way of telling us that it is healing, and people that suffer more initial discomfort often achieve the greatest long-term results.